Prostate health and sexual function are deeply connected, but many men don’t realize how much this small gland can influence erections, ejaculation, orgasm, and even desire. When the prostate is irritated, enlarged, infected, or treated for cancer, the impact is rarely limited to urination alone – the entire sexual system can be affected.
This article explains in clear, medically grounded detail how prostate health affects sexual function, what is happening inside the body, and why changes in the prostate often show up first in the bedroom.
A quick look at the prostate’s role in sex
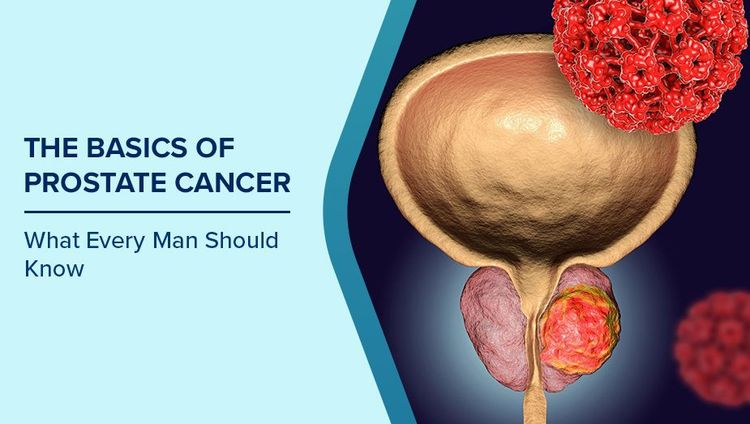
The prostate is a walnut-sized gland located just below the bladder, wrapping around the urethra (the tube carrying urine and semen out of the body).
It contributes to sexual function by:
- Producing 30–40% of semen volume
- Secreting fluid that nourishes and protects sperm
- Helping create the force of ejaculation by rhythmic muscle contractions
- Sitting very close to nerves and blood vessels that are crucial for erections and orgasm
Because of this anatomy, anything that disturbs the prostate – inflammation, enlargement, surgery, radiation, or hormone changes – can disturb the delicate coordination required for normal sexual function.
How prostatitis affects sexual function
Prostatitis is inflammation of the prostate, often causing pelvic pain, urinary symptoms, and sexual discomfort. It may be bacterial (infection) or non-bacterial (chronic pelvic pain syndrome).
Ways prostatitis can affect sex:
- Painful ejaculation
Inflammation makes the prostate and surrounding tissues hypersensitive; when the gland contracts during orgasm, it can cause sharp or burning pain instead of pleasure. - Decreased libido
Persistent pain, fatigue, and anxiety can reduce sexual desire, even when hormone levels are normal. - Erectile difficulties
Pain and psychological stress (fear of pain, performance anxiety) can make it hard to get or keep an erection. - Shortened or weaker orgasm
If the prostate cannot contract normally, ejaculation may feel weak, incomplete, or less satisfying.
The good news: when prostatitis is correctly treated (antibiotics if bacterial, pelvic floor therapy, anti-inflammatory measures, stress management), many men see significant improvement in both symptoms and sexual performance.
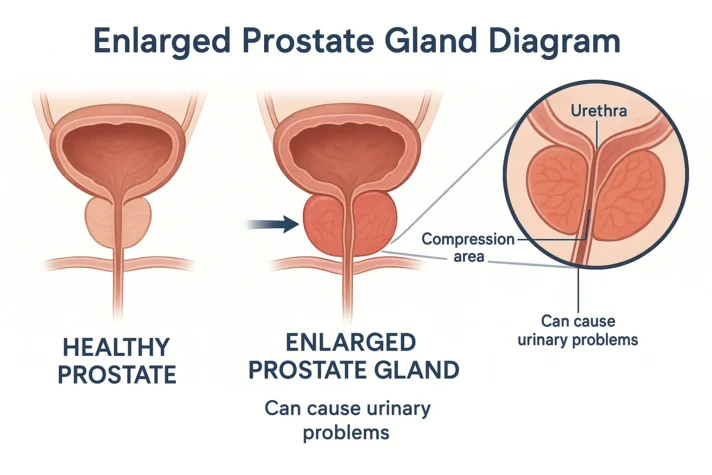
How BPH (Enlarged Prostate) affects sexual function
Benign Prostatic Hyperplasia (BPH) is a non-cancerous enlargement of the prostate, common in men over 50. Its hallmark symptoms are urinary: slow stream, hesitancy, dribbling, frequent urination, especially at night.
However, BPH also affects sexual function in several ways:
- Lower urinary tract symptoms (LUTS) and erections
Research shows a strong association between moderate/severe urinary symptoms and erectile dysfunction (ED). Constant urgency, interrupted sleep, and discomfort weaken energy, confidence, and mood, all of which are important for sexual performance. - Reduced ejaculation volume
As the prostate enlarges, the pattern of fluid flow can change, and some men notice less semen or a weaker ejaculation. - “Dry” or retrograde ejaculation
Some BPH medications (especially certain alpha-blockers) relax the bladder neck so much that semen flows backward into the bladder during orgasm instead of out through the urethra. This is not dangerous, but it can feel strange or unsatisfying and may affect fertility. - Psychological impact on libido
Worrying about urinary accidents, odour, or frequent trips to the bathroom can make men avoid intimacy, which then reduces desire and sexual frequency over time.
Medications for BPH can also influence sexual function:
- Alpha-blockers (tamsulosin, etc.):
May cause retrograde ejaculation but usually have less impact on erectile function. - 5-alpha reductase inhibitors (finasteride, dutasteride):
Can reduce DHT (a potent androgen), sometimes leading to decreased libido, weaker erections, or reduced semen volume in a subset of men.
Not every man experiences these side effects, but it is important to be aware and speak with a clinician if changes in sexual function occur after starting treatment.
How prostate cancer and its treatments affect sexual function
Prostate cancer itself, especially in early stages, often does not cause sexual symptoms. Many men are diagnosed by elevated PSA or abnormal digital rectal exam while still sexually active.
However, treatments for prostate cancer frequently affect sexual function:
Radical prostatectomy (surgical removal of the prostate)
- The prostate and seminal vesicles are removed; the urethra is reconnected to the bladder.
- Nerves responsible for erections run very close to the prostate.
Even with “nerve-sparing” techniques, these nerves can be stretched, bruised, or partially damaged.
Possible consequences:
- Erectile dysfunction
Ranges from temporary to long-term, depending on age, pre-surgery function, and surgical technique. - Dry ejaculation (no semen)
Because the prostate and seminal vesicles are removed, orgasm occurs without ejaculate, which can be surprising even though the pleasure of orgasm may still be present. - Changes in orgasm quality
Some men describe orgasms as shorter, less intense, or experienced differently after surgery.
Radiation therapy
Radiation to the prostate (external beam or brachytherapy) can:
- Damage blood vessels and erectile nerves gradually
- Lead to erectile dysfunction that develops months or years after treatment
- Cause dry or reduced semen volume

Hormone therapy (Androgen Deprivation Therapy – ADT)
Hormone therapy drastically reduces levels of testosterone and DHT to slow cancer growth.
Effects on sexual function include:
- Profound loss of libido
- Difficulty or inability to achieve erection
- Decreased semen production and infertility
- Emotional changes (low mood, fatigue) that further reduce sexual interest
These changes are substantial but often predictable and can be partly managed with counseling, lifestyle optimization, and, in some cases, medications or devices for erectile support.
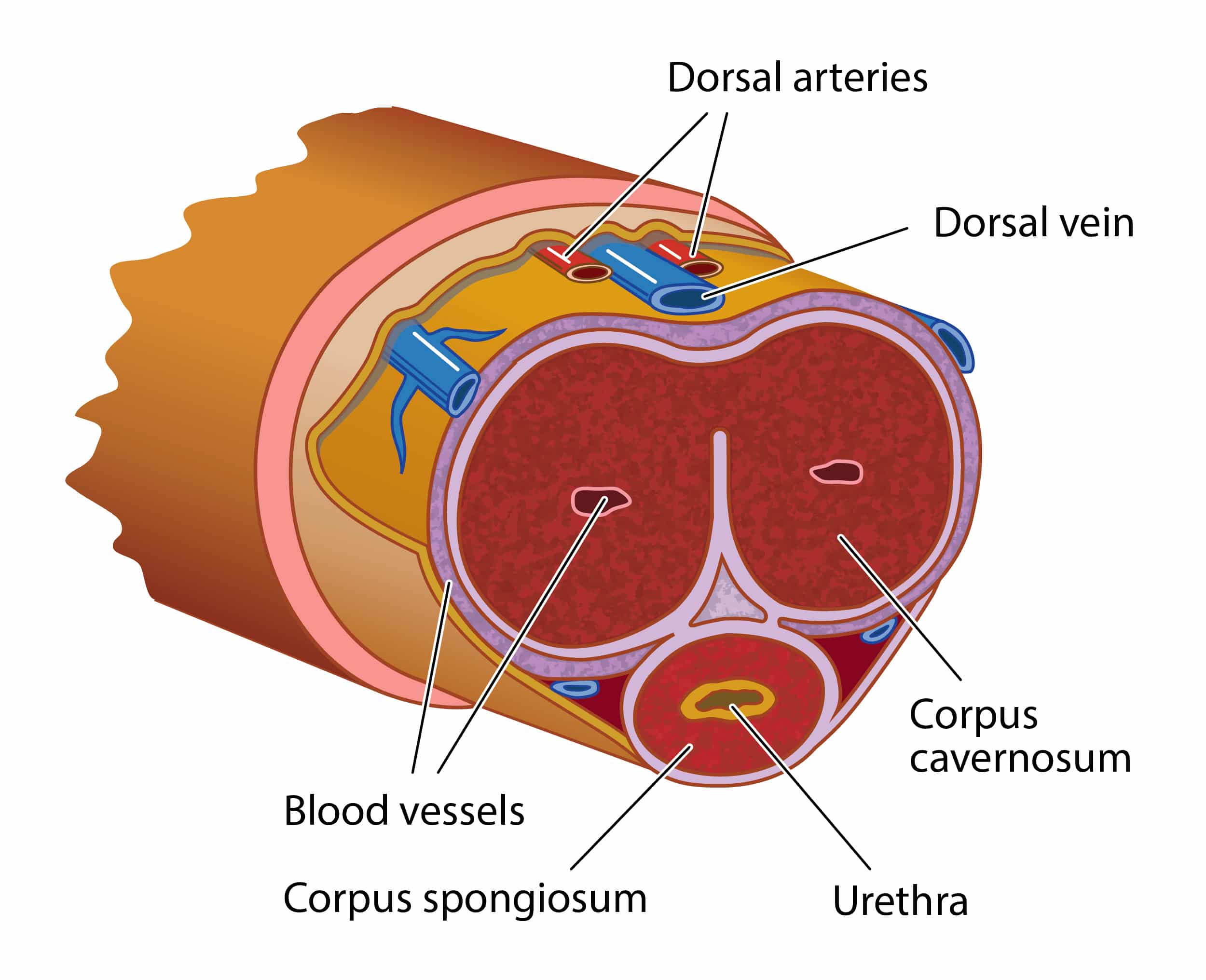
Nerve and blood flow: the critical link between prostate and erections
The nerves that control erection (cavernous nerves) run alongside the prostate and pass through the pelvic region. The arteries supplying blood to the penis also pass close to the gland.
When the prostate is:
- Inflamed (prostatitis)
- Enlarged and compressing surrounding structures (BPH)
- Surgically removed or irradiated (cancer treatment)
…these nerves and vessels can be directly or indirectly affected.
Results may include:
- Slower or weaker erections
- Need for more stimulation to become aroused
- Difficulty maintaining erections until orgasm
This is why erectile dysfunction and prostate disease often appear together, especially in older men.
Pain, anxiety, and the mind–body loop
Beyond anatomy, prostate issues strongly influence psychological well-being, which in turn affects sexual function.
Common emotional effects:
- Fear that urinary or sexual symptoms mean cancer
- Embarrassment about urinary frequency or leakage
- Anxiety about performance or disappointing a partner
- Depression due to chronic pain or loss of sexual confidence
These mental states can:
- Suppress libido
- Make it harder to get an erection, even if the nerves and vessels are intact
- Lead to avoidance of intimacy and reduced relationship satisfaction
Addressing both medical and psychological aspects is crucial for restoring healthy sexual function.
Can improving prostate health improve sexual function?
In many cases, yes.
- Treating prostatitis can reduce pain and restore normal ejaculation and erections.
- Managing BPH can improve sleep, reduce urinary urgency, and renew confidence, which often boosts sexual interest and performance.
- For men after prostate cancer treatment, early rehabilitation of erections (medications, vacuum devices, pelvic floor exercises, lifestyle changes) can help maximize recovery.
Supporting strategies that benefit both prostate and sexual function include:
- Maintaining a healthy weight and waistline
- Regular physical activity (especially cardio + strength training)
- A diet rich in vegetables, fruits, healthy fats, and low in processed foods
- Limiting alcohol and avoiding smoking
- Managing stress and prioritizing sleep
- Open communication with partners and healthcare professionals
When to see a doctor
Men should seek medical evaluation if they notice:
- Persistent urinary symptoms (weak stream, urgency, frequent night urination)
- Pain in the pelvis, perineum, or during ejaculation
- New or worsening erectile problems
- Blood in urine or semen
- Significant change in ejaculation volume or pattern without clear cause
Early consultation allows for proper diagnosis – distinguishing between prostatitis, BPH, and prostate cancer – and choosing treatment options that consider both prostate health and sexual function.
Prostate health is not just about urination or cancer risk; it is deeply tied to sexual satisfaction, intimacy, and quality of life. Understanding this connection empowers men to address symptoms early, discuss openly with their partners and doctors, and protect both their prostate and their sexual well-being.