Prostate conditions are extremely common in men, especially after the age of 40. Yet prostatitis, BPH (Benign Prostatic Hyperplasia), and prostate cancer are often misunderstood because they can share similar urinary symptoms. Despite this overlap, these conditions are medically distinct, each with its own cause, risk pattern, diagnostic markers, and treatment approach.
Understanding the differences helps men recognize symptoms early, reduce anxiety, and seek the correct medical intervention.
What Is Prostatitis?
Prostatitis refers to inflammation of the prostate, which can be caused by infection (bacterial prostatitis) or occur without infection (chronic prostatitis/chronic pelvic pain syndrome).
Key characteristics
- Often affects younger or middle-aged men
- Can appear suddenly (acute) or persist for months (chronic)
- Symptoms relate more to pain and discomfort than prostate enlargement
Common symptoms
- Pelvic, groin, or lower back pain
- Pain during urination or ejaculation
- Frequent urination, especially at night
- Burning sensation when urinating
- Sometimes fever or chills (if bacterial)
Causes
- Bacterial infection (E. coli is most common)
- Pelvic floor muscle tension
- Stress-related pain
- Urinary tract dysfunction
- Post-viral inflammation
Diagnosis
- Urine culture
- Prostate exam (tender, warm prostate)
- Semen analysis in some cases
Treatment
- Antibiotics for bacterial cases
- Anti-inflammatory medications
- Pelvic floor therapy
- Alpha-blockers
- Lifestyle adjustments (stress reduction, heat therapy)
Prostatitis is not related to cancer and does not increase prostate cancer risk, but symptoms may mimic other conditions.
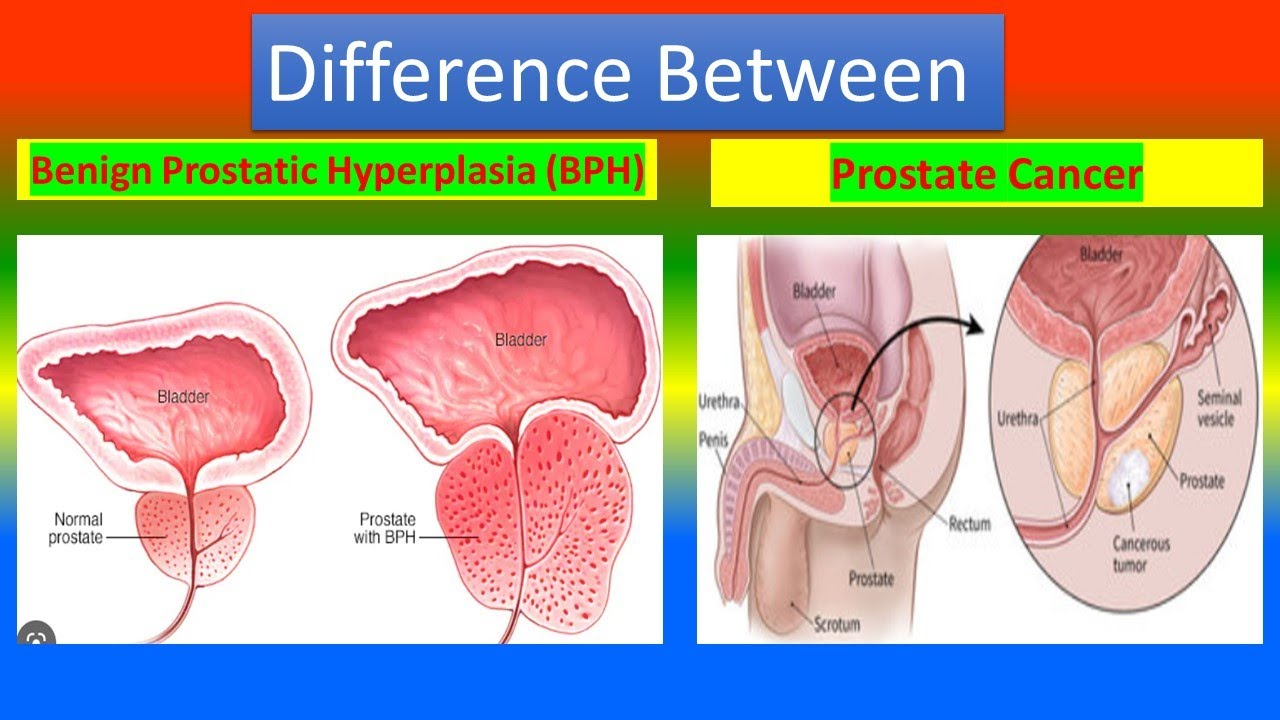
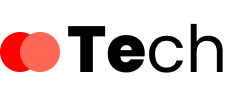
What Is BPH (Benign Prostatic Hyperplasia)?
BPH is non-cancerous enlargement of the prostate commonly seen in aging men. As the prostate grows, it compresses the urethra, leading to urinary obstruction.
Key characteristics
- Very common in men over 50
- Caused by hormonal changes (especially DHT)
- Symptoms arise from mechanical blockage of urine flow
Common symptoms
- Weak urine stream
- Difficulty starting urination
- Frequent urination
- Urgency or dribbling
- Waking up repeatedly at night to urinate
- Feeling of incomplete bladder emptying
Causes
- Age-related hormonal shifts (DHT accumulation)
- Prostate cell growth imbalance
- Genetics and metabolic factors
Diagnosis
- Digital Rectal Exam (DRE)
- PSA blood test
- Ultrasound or prostate volume measurement
- Uroflowmetry (urine flow study)
Treatment
- Alpha-blockers (relax prostate muscles)
- 5-alpha reductase inhibitors (shrink the prostate)
- Combination therapy
- Minimally invasive procedures (Rezum, UroLift)
- Surgery for severe obstruction (TURP, HoLEP)
BPH is not cancer and does not turn into cancer, but enlarged prostate can elevate PSA levels, requiring proper evaluation.
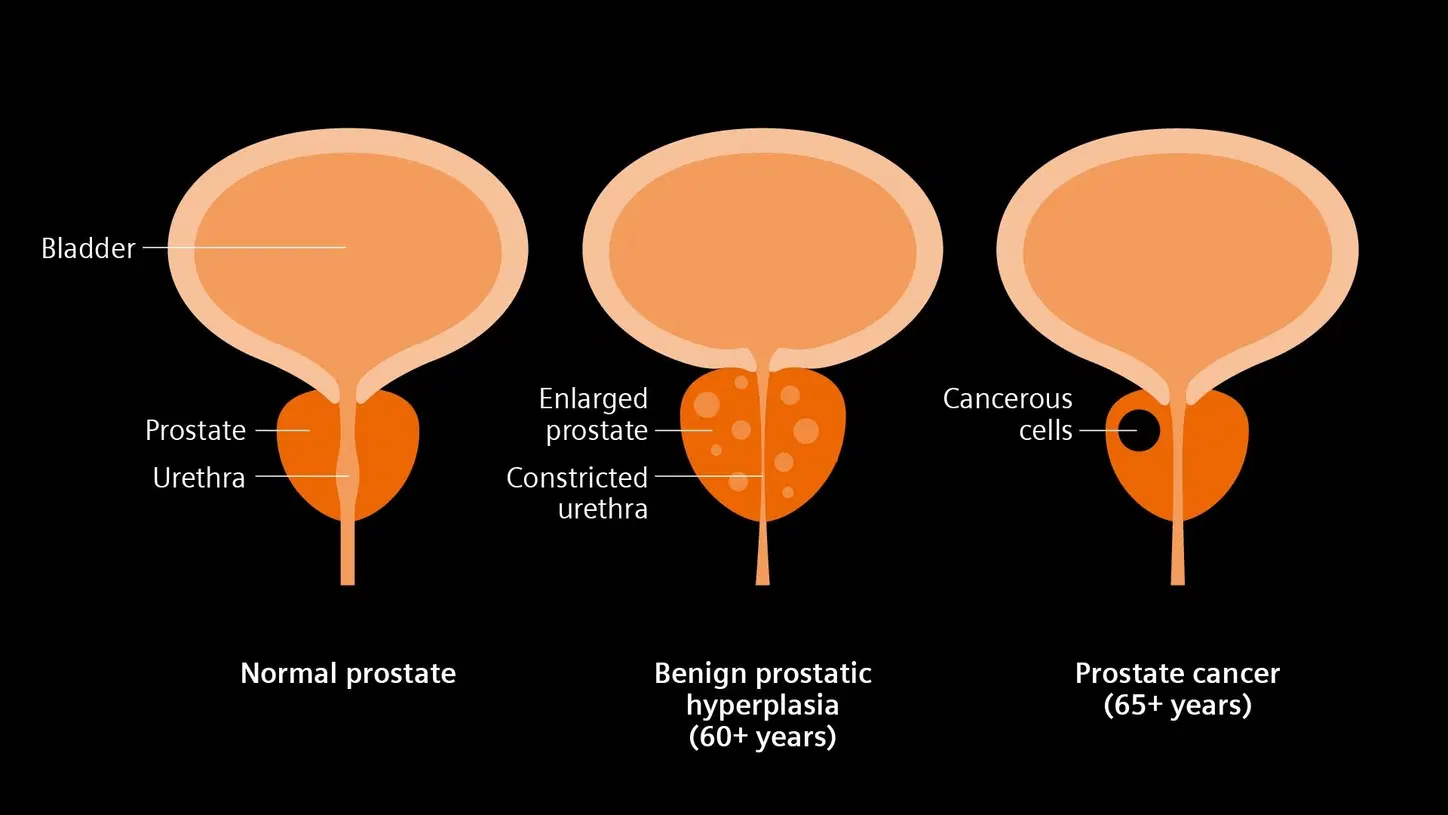
What Is Prostate Cancer?
Prostate cancer occurs when cells in the prostate grow uncontrollably. It is one of the most common cancers in men, especially those over 60.
Key characteristics
- Often slow-growing, but some forms are aggressive
- Early stages may show no symptoms
- Strongly linked to age, genetics, and lifestyle factors
Common symptoms (usually in later stages)
- Difficulty urinating
- Blood in urine or semen
- Bone pain (if cancer spreads)
- Unintentional weight loss
- Weak urine flow
Because early-stage prostate cancer rarely causes symptoms, screening is crucial.
Causes and risk factors
- Age over 55
- Family history of prostate cancer
- African ancestry
- High-fat diets
- Obesity
- Low physical activity
Diagnosis
- PSA test (Prostate-Specific Antigen)
- DRE
- MRI
- Prostate biopsy (definitive diagnosis)
Treatment
Depends on risk level:
- Active surveillance (for slow-growing cancer)
- Surgery (prostatectomy)
- Radiation therapy
- Hormone therapy (reduces testosterone)
- Chemotherapy
- Targeted therapy / immunotherapy for advanced cases
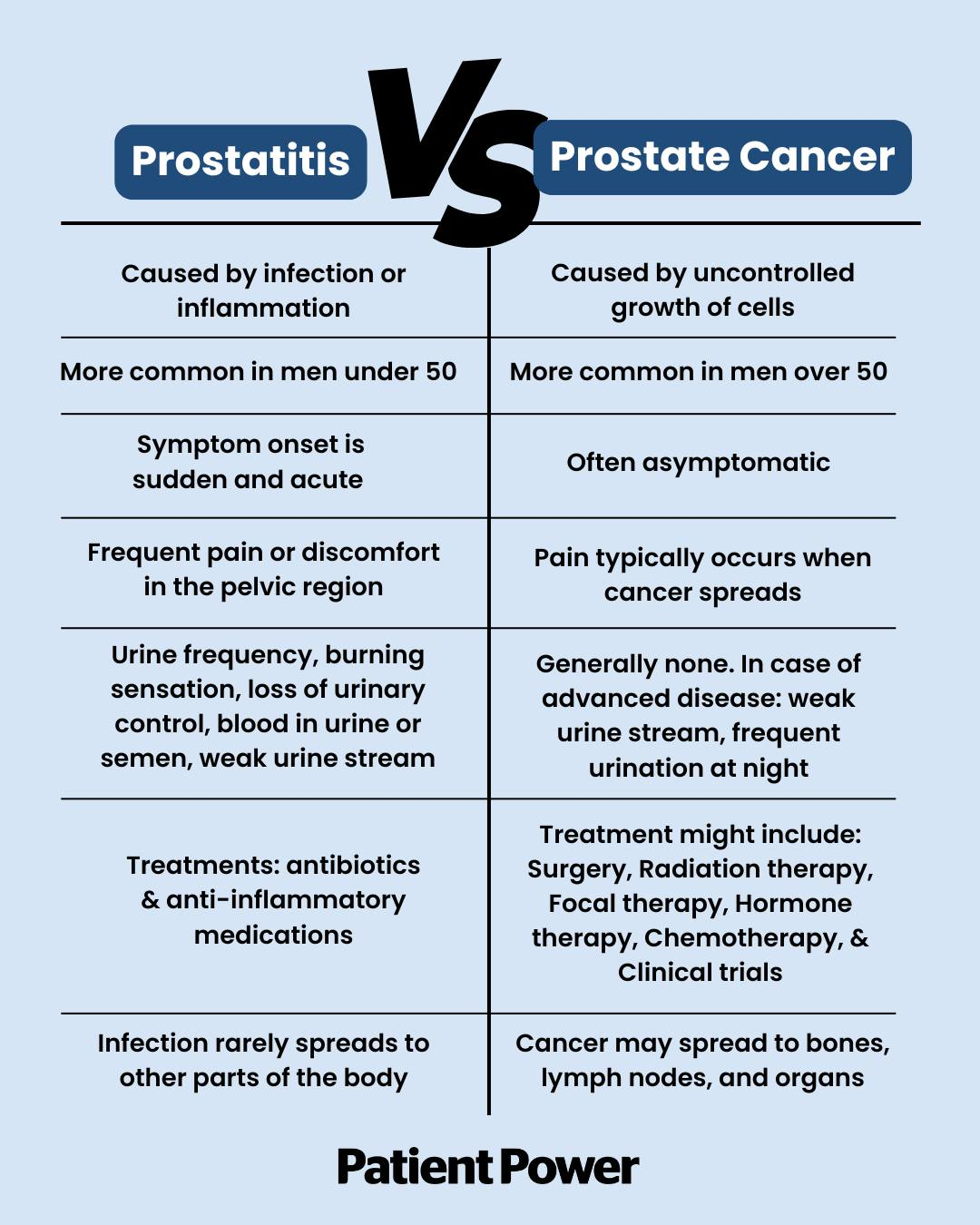
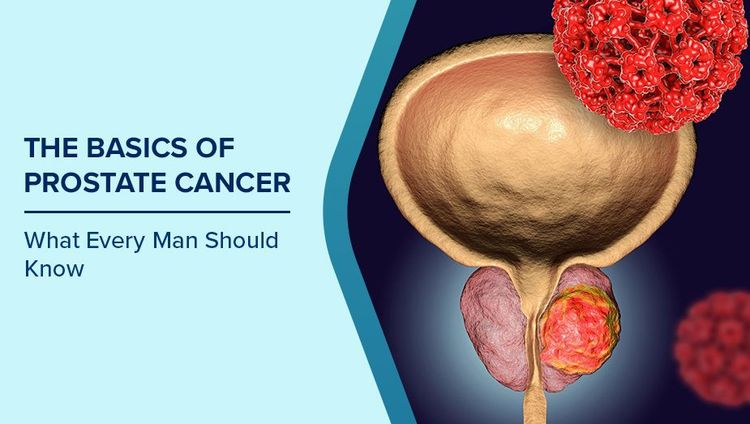
How to Tell the Difference: Prostatitis vs. BPH vs. Prostate Cancer
Symptoms comparison
| Feature | Prostatitis | BPH | Prostate Cancer |
|---|---|---|---|
| Age group | 20–50 | 50+ | 55+ |
| Pain | Very common | Rare | Rare (except advanced stages) |
| Fever | Possible (acute) | No | No |
| Urinary symptoms | Common | Very common | Common (late) |
| Onset | Sudden or chronic | Gradual | Often silent |
| PSA level | Can be high | Can be high | Often high |
Key distinctions
- Prostatitis → pain + inflammation, often in younger men
- BPH → prostate enlargement + urinary blockage, in older men
- Prostate cancer → abnormal cell growth, often silent until advanced
If a man experiences urinary symptoms, elevated PSA, or unexplained pelvic discomfort, a medical evaluation is essential to confirm the correct condition.
Which Condition Is the Most Serious?
- Prostatitis – uncomfortable but treatable; not life-threatening
- BPH – benign but can severely affect quality of life if untreated
- Prostate cancer – potentially life-threatening, especially if detected late
Early diagnosis makes a significant difference in treatment success.
Conclusion
Although prostatitis, BPH, and prostate cancer may share similar urinary symptoms, they differ fundamentally in cause, age of onset, severity, and treatment approach. Recognizing these differences helps men take timely action, reduce misinterpretation of symptoms, and seek the right medical guidance.