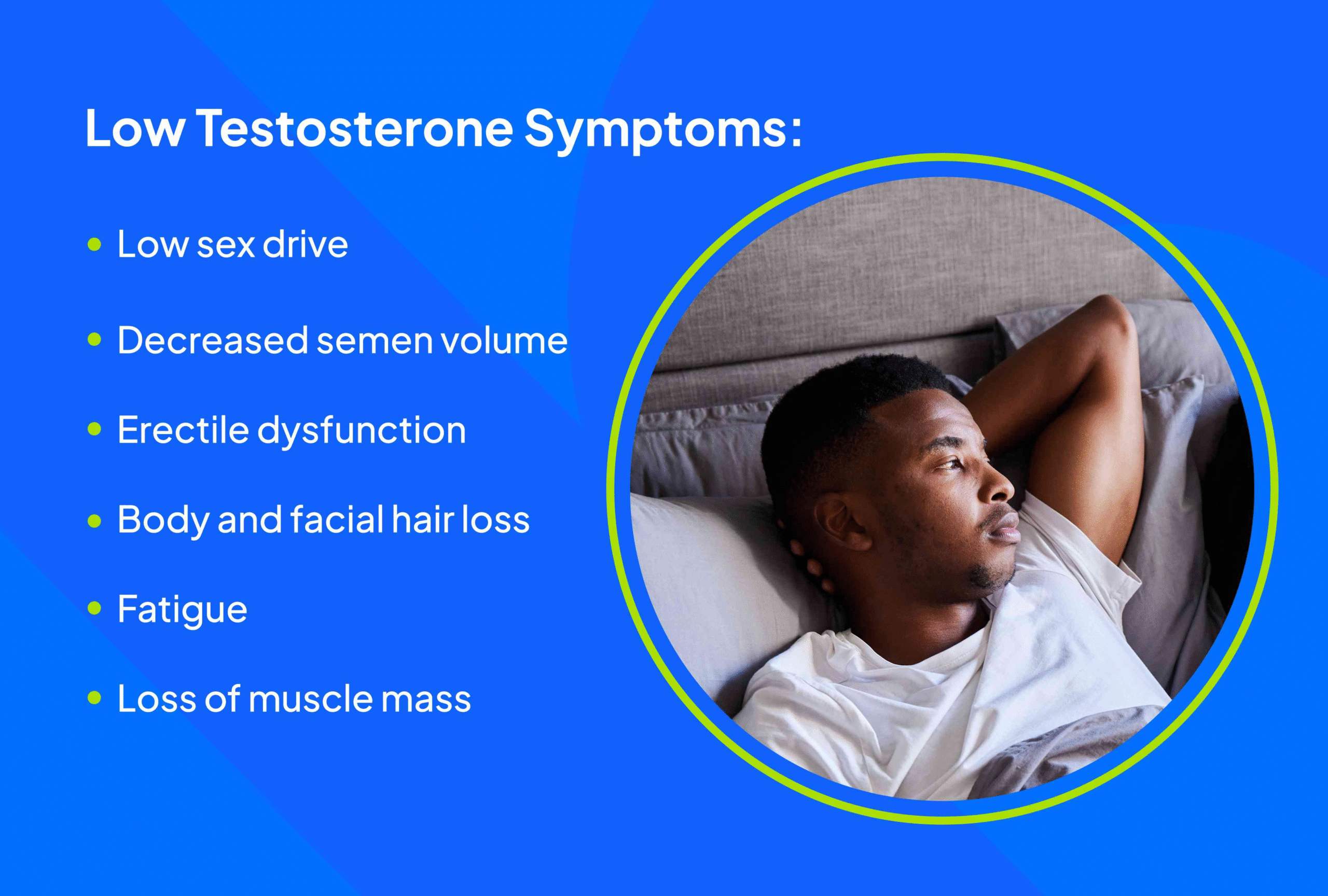
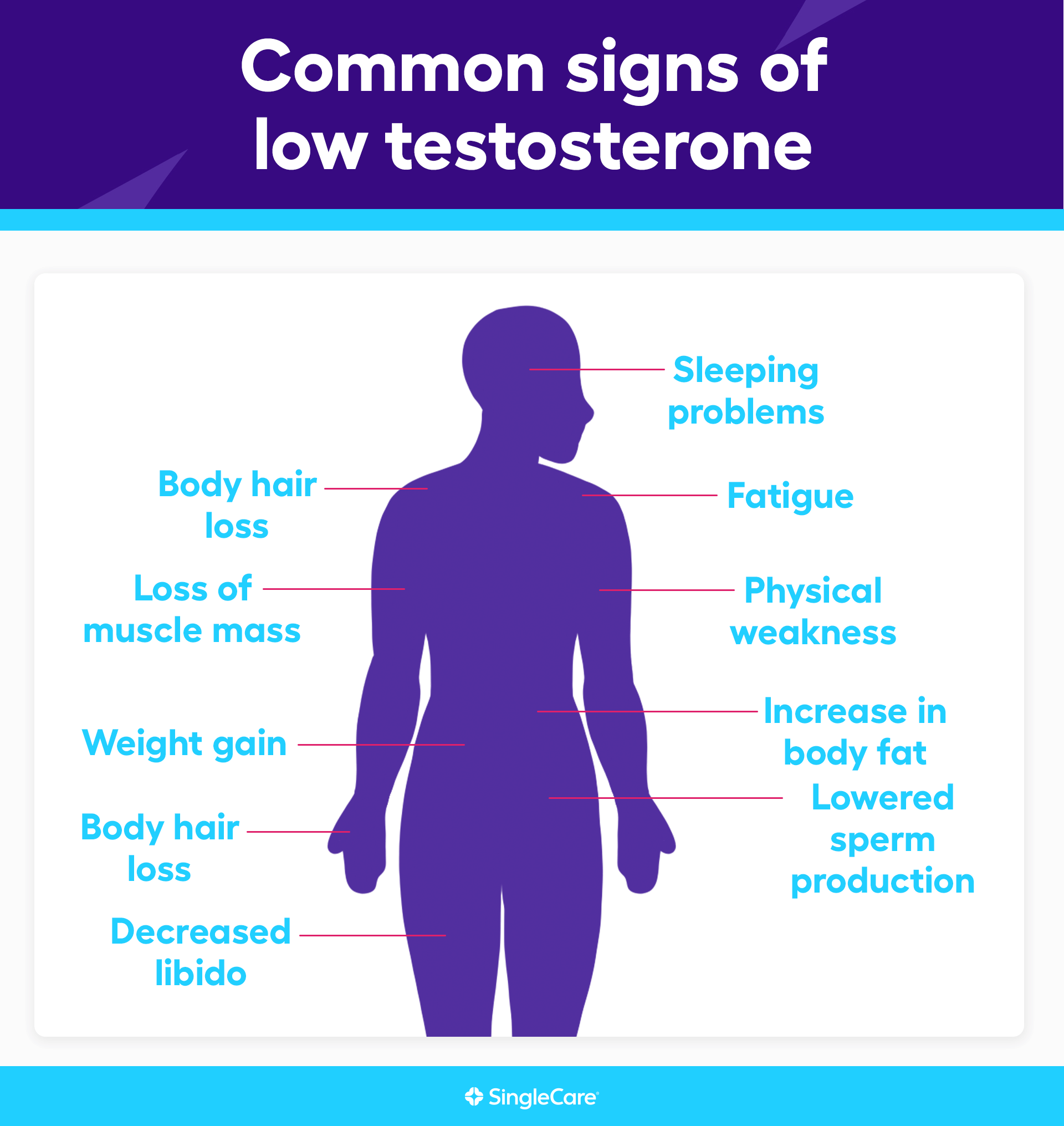
Low testosterone (also known as Hypogonadism) is a condition in which the testes do not produce enough testosterone, the primary male sex hormone responsible for sexual function, muscle mass, bone density, red blood cell production, and overall well-being. Testosterone levels naturally decline with age, but many men experience a drop earlier or more severely due to underlying medical conditions, lifestyle factors, or disruptions in the hormonal regulatory system.
Below are the main medically recognized causes of low testosterone in men.
1. Age-related hormonal decline (Andropause)
Testosterone decreases approximately 1–2% per year after the age of 30.
This decline occurs because:
- Leydig cells in the testes lose efficiency.
- The pituitary gland reduces LH (Luteinizing Hormone) secretion.
- The hypothalamus becomes less sensitive to hormonal feedback.
Although age-related decline is natural, symptoms vary significantly among individuals.
2. Primary testicular failure (Primary Hypogonadism)
In this form, the testes themselves cannot produce adequate testosterone despite adequate stimulation from the brain.
Major causes include:
- Genetic disorders:
- Klinefelter syndrome (XXY)
- Undescended testes (cryptorchidism)
- Testicular injury or trauma
Physical damage reduces functional testicular tissue. - Infections
- Mumps orchitis (post-puberty)
- Severe epididymo-orchitis
- Chemotherapy or radiation therapy
These treatments can permanently impair Leydig cell function. - Testicular torsion or vascular issues
Loss of blood flow leads to irreversible damage.
Men with primary hypogonadism often have high LH and FSH levels because the brain tries to stimulate the testes but receives no response.
3. Secondary hypogonadism (Pituitary or Hypothalamic dysfunction)
Here, the testes are healthy but do not receive enough hormonal signals from the brain.
Key medical causes:
- Pituitary tumors (adenomas)
Tumors can impair LH and FSH secretion.
Prolactin-secreting tumors (prolactinomas) are a common cause. - Hypothalamic disorders
- Kallmann syndrome
- Trauma
- Brain surgery
- Congenital GnRH deficiency
- Systemic illnesses
Chronic diseases can suppress the hypothalamic–pituitary–gonadal (HPG) axis.
Common systemic contributors include:
- Chronic kidney disease
- Liver cirrhosis
- HIV/AIDS
- Severe hypothyroidism
- Uncontrolled diabetes
In secondary hypogonadism, LH and FSH are low or inappropriately normal despite low testosterone.
4. Obesity and metabolic syndrome
Among modern men, obesity is one of the most common causes of low testosterone.
Mechanisms include:
- Increased aromatase activity → converts testosterone into estrogen.
- Insulin resistance → disrupts LH secretion from the pituitary.
- Chronic inflammation → impairs Leydig cell function.
- Excess body fat stores and lowers free testosterone levels.
Men with central obesity often have normal total testosterone but low free testosterone, which leads to symptoms.
5. Medications that suppress testosterone
Several drugs directly or indirectly reduce testosterone production:
- Opioids (morphine, oxycodone, tramadol): inhibit the HPG axis.
- Glucocorticoids (prednisone): suppress hypothalamic hormone release.
- Anabolic steroid abuse: shuts down natural testosterone production.
- Chemotherapy agents
- Antidepressants (some SSRIs may affect libido/hormones indirectly).
- Ketoconazole (an antifungal that blocks steroid synthesis).
- Spironolactone (anti-androgenic effects).
Men taking long-term medications should be evaluated if symptoms develop.
6. Chronic stress and elevated cortisol
High cortisol suppresses testosterone at multiple levels:
- Reduces GnRH release from the hypothalamus
- Lowers LH secretion
- Directly inhibits testicular testosterone synthesis
Chronic psychological stress, sleep deprivation, and anxiety disorders can significantly depress testosterone levels.
7. Sleep disorders (especially sleep apnea)
Testosterone production peaks during deep sleep.
Men with obstructive sleep apnea often have reduced testosterone due to:
- Fragmented sleep
- Reduced REM cycles
- Hypoxia (low oxygen levels)
Treating sleep apnea often improves hormone levels without medication.
8. Excessive alcohol consumption
Alcohol damages Leydig cells, disrupts LH secretion, and increases estrogen through liver dysfunction.
Chronic alcohol use may cause:
- Testicular atrophy
- Reduced sperm production
- Low testosterone symptoms (fatigue, low libido, poor erections)
9. Inflammation and autoimmune diseases
Conditions such as:
- Sarcoidosis
- Hemochromatosis
- Autoimmune orchitis
can impair both testicular and pituitary functions, leading to hypogonadism.
10. Nutritional deficiencies and poor lifestyle
Low levels of essential nutrients affect testosterone synthesis:
- Zinc deficiency
- Vitamin D deficiency
- Low magnesium
- Protein-restricted diets
Sedentary lifestyle, excessive heat exposure on the testes (sauna, hot tubs), and lack of resistance training also lower testosterone over time.
Conclusion: Low Testosterone Has Many Causes — Medical Evaluation Is Essential
Low testosterone in men can result from testicular damage, pituitary dysfunction, chronic disease, obesity, stress, medications, or age-related decline. Because the causes are diverse and sometimes serious, a proper medical evaluation—including blood tests for Total Testosterone, Free Testosterone, LH, FSH, Prolactin, and Thyroid function—is crucial for accurate diagnosis.
Understanding the root cause helps determine whether treatment requires lifestyle changes, management of underlying disease, medication adjustment, or Testosterone Replacement Therapy (TRT).